1. What is the difference between Cushing’s Syndrome and Cushing’s Disease?
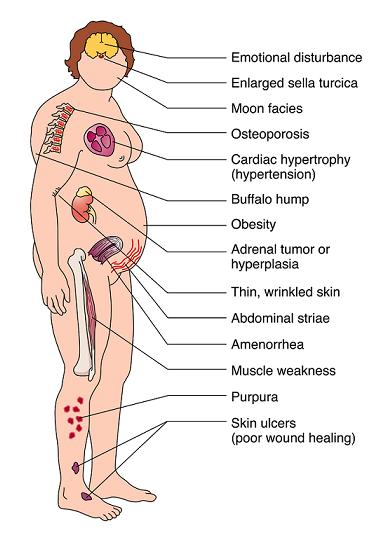
Any condition that causes the adrenal gland to produce excessive
cortisol results in the disorder Cushing’s syndrome. Cushing’s syndrome
is characterized by facial and torso obesity, high blood pressure,
stretch marks on the belly, weakness, osteoporosis, and facial hair
growth in females.
Cushing’s syndrome has many possible causes including tumors within
the adrenal gland, adrenal gland stimulating hormone (ACTH) produced
from cancer such as lung cancer, and ACTH excessively produced from a
pituitary tumors within the brain. ACTH is normally produced by the
pituitary gland (located in the center of the brain) to stimulate the
adrenal glands’ natural production of cortisol, especially in times of
stress.
When a pituitary tumor secretes excessive ACTH, the disorder
resulting from this specific form of Cushing’s syndrome is referred to
as Cushing’s Disease.
As an aside, it should be noted that doctors will sometimes describe
certain patients with features identical to Cushing’s syndrome as having
‘Cushingoid’ features. Typically, these features are occurring as side
effects of cortisone-related medications, such as prednisone and
prednisolone.
2. What is cortisol?
Cushing’s syndrome, or hypercortisolism, occurs when the body’s tissues are exposed to too much of the hormone cortisol.
In a healthy person, cortisol is a hormone pumped out every day by
the adrenal cortex. The adrenal glands sit atop the kidneys. Cortisol
assists the body to deal with various stresses. It reduces inflammation
and immune system function and triggers the breakdown of protein into
sugars. The pituitary gland, which lies just beneath the brain, sends
the signal that triggers cortisol production, with the peak output
occurring around 8 a.m. — as if nature were providing a jolt to get
moving.
At normal levels, 25 micrograms per deciliter of blood in the morning
and about 5 micrograms at night, cortisol is essential to life. It
helps regulate blood pressure, energy production, the ability to fight
infections and respond to stress. It also seems to keep the immune
system in check so that it doesn’t make antibodies that might attack the
body’s own tissues. And it seems to balance the effects of insulin in
breaking down sugar for energy and to regulate the metabolism of
proteins, carbohydrates and fats.
A certain amount of cortisol is necessary for life. Without cortisol
even a small amount of stress will kill you. Addison’s disease, which
President John F. Kennedy had, is a disease which causes low cortisol
levels, and which is treated by cortisol replacement therapy.
But too much cortisol — whether produced naturally in the body or
taken as steroids — is disastrous, too. It can cause sudden weight gain,
especially in the trunk, a florid moon-like face, thin skin, mood
changes, muscle weakness, purple stretch marks on the torso, high blood
pressure, diabetes, a fatty “buffalo” hump on the neck, depression, and
severe osteoporosis.
3. Is pituitary surgery the only cure for Cushing’s Disease?
Yes. Researchers are currently doing clinical trials with
medications, but the use of that medicine to cure Cushing’s could be
years and years away.
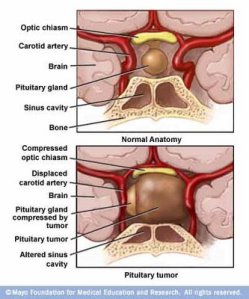
4. What does the pituitary look like with a tumor in it?
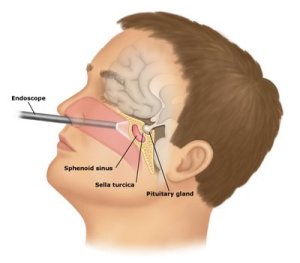
5. What is involved in pituitary surgery?
Neurosurgeons access the pituitary gland through the nose or under
the lip, called endoscopic endonasal transsphenoidal surgery. Using an
endoscope with a camera attached, surgeons enter a patient’s nose and
sinuses, allowing them to approach the tumor without any external
incisions. Guided by the endoscope and enhanced computer navigation,
surgeons open small holes in the base of the skull and membrane covering
the brain to remove the tumor. Better visualization and access to these
lesions have enabled improved resection of the tumor without causing
damage to the brain and lower risk of complications and follow up
surgery. This results in surgery with a shorter hospital stay, a faster
recovery and improved outcomes.
6. How long does it take to recover from pituitary surgery?
Recovery from pituitary surgery is a long battle. It varies from
patient to patient and is directly related to the length of time you’ve
had Cushing’s because of the damage that high cortisol does to the
body’s systems. It can take 12-18 months before the patient returns to
“normal” and that is only if further pituitary surgeries and procedures
are not needed.
Once the tumor is removed from the pituitary, the body switches from
producing too much cortisol to not producing enough. Cortisol
supplements are taken to replace the off-kilter cortisol production.
This must be taken not only on a daily and timed basis but also in
certain situations: sickness and stress (good or bad). Cortisol
supplements are taken after surgery to replicate the patient’s normal
hormonal production. Each week, the patient reduces the amount of
cortisol replacements. If the patient experiences terrible symptoms
associated with adrenal insufficiency, then the patient must temporarily
increase the amount of cortisol replacement hormones he/she takes and
often go to the emergency room. This process varies from person to
person, and it makes recovery very difficult for the patient.
7. Once you have surgery, are you cured?
Not necessarily. The pituitary is so small (less than 2 cm), and the
tumors are so small, that the neurosurgeon does his best to remove all
of the cells that are producing too much ACTH. In 60% of the cases, the
surgeon succeeds. In 40% of the cases, he doesn’t. For some patients,
several surgeries are needed to try to remove all the cells. A patient
may choose to have a bilateral adrenalectomy, the removal of both
adrenal glands. This surgery is performed after two pituitary surgeries
fail to remove all of the tumor(s) present. The pituitary tumors secrete
ACTH which stimulates the adrenals to produce cortisol. Since a surgeon
does not want to remove all of the pituitary gland–as it controls many
other vital hormones that the body needs–many opt for the final road to
end Cushing’s, which is to remove both adrenal glands. These glands are
responsible for the production of cortisol, and removing these glands is
the only permanent way to end cortisol production once and for all.
However, due to the important life-saving functions of cortisol, the
patient must take cortisol medicine in pill form for the rest of his/her
life.
However, it is not as simple as popping a pill every day. Let’s
compare a Cushing’s patient post BLA with a Type I diabetic. Stress
management for Cushing’s patients is just as critically important as
blood sugar management is for diabetics.
A diabetic must look at a plate of food, estimate the amount of
carbohydrates contained therein, and take insulin for that amount of
carbohydrates (which calculations are often aided by the nutritional
facts on the packaging).
A Cushing’s patient post BLA must take cortisol replacement medicine
in response to the amount of ‘sickness’ or ‘stress.’ These events are
unquantifiable and lack data on packaging. In addition, there is not a
day goes by without stress or challenges of some sort. These episodes
can prove challenging for a Cushing’s patient in determining how much
medicine to take to offset these challenges. This makes it difficult for
the Cushing’s patient to fully return to his/her lifestyle before
Cushing’s.
8. Does a pituitary tumor shorten life?
Having a pituitary tumor should not shorten life if it is properly
treated and if the patient receives appropriate hormone replacement. All
medications must be taken as directed. Additionally, there is a need
for regular medical care and monitoring of medical treatments. Most
patients who have had a pituitary tumor engage in normal work and social
activities. If a patient requires steroid (cortisol) replacement, a
“medic alert” bracelet or necklace should be worn at all times. Another
illness such as the flu, pneumonia or an accident requires an increase
in the steroid dose. If the patient is brought to the hospital and
unable to give the medical history, the physicians will have no way of
knowing that additional steroid is necessary. Thus, with attention to
these important details, a patient with a pituitary tumor should have a
full and productive life.
9. Is a pituitary tumor cancer?
No, in over 99% of patients, this is NOT a cancer; it is benign.
Although the tumor is benign, it can cause problems because of its size,
because it causes the normal pituitary gland to become underactive
(hypopituitarism) or because of excessive hormone production by the
tumor.
10. Can stress cause Cushings Syndrome?
No. Stress-related increased cortisol production by the adrenal
glands is normal and physiological, and does not lead to Cushing’s
syndrome. It can be produced by prolonged, high doses of corticosteroid
medications and can also result from adrenal gland tumors producing
abnormally excessive amounts of cortisol. One other cause is excessive
stimulation of the adrenal glands to produce cortisol by high levels of
ACTH hormones secreted by a diseased pituitary gland or other abnormal
glands.
11. Can my family doctor/primary care physician detect high cortisol levels?
Yes. Your primary care physician can take the first step in
diagnosing Cushings with a simple 24 hour urine free cortisol test.
However, most doctors (in my personal experience as well) do not know to
look for high cortisol levels, so unfortunately, the patient must
specifically request the test from a regular family physician. If the
results do come back high, they may refer you to an endocrinologist. If
they do not come back abnormal, this does not mean you do not have
Cushings. Cortisol levels fluctuate, so if other symptoms do exist and
even more, PERSIST, insist that you see a specialist. You may have to
take your healthcare into your own hands, but get the help you know you
need and deserve.